What is Breast Cancer?
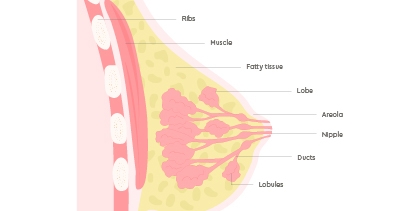
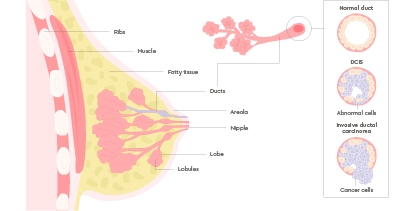
Breast cancer starts when normal breast cells acquire mutations leading to uncontrolled growth, creating a tumour. It often begins in the cells that line the milk ducts (ductal cancer) but can also arise in the glands that make milk, called breast lobules (lobular cancer).
Invasive breast cancer is when the tumour grows into the surrounding breast tissue. Cancer cells have the potential to break away and initially spread to the lymph glands, and at a later stage spread elsewhere in the body, which is called secondary breast cancer.
Anyone (including men) can get breast cancer, as we all have some breast tissue. Four in five cases are in women older than 50 and your risk increases as you age. The earlier it’s found, the easier it is to treat, so we encourage everyone to know their breasts.
Call us today
Early signs and symptoms
Getting to know how your breasts normally look and feel means you can spot any changes that could be breast cancer symptoms. Experts recommend checking your breasts once a month.
Breast cancer isn’t always a lump, so make sure you know all the signs
What does breast cancer look like?
Stand in front of a mirror and compare one breast to the other.
Look out for:
- Skin changes – thickening, rashes, or many small pinprick dimples like orange peel (peau d’orange)
- Colour changes in your skin or nipples such as redness if you have white skin, or darkening if you have brown or black skin
- Appearance – changes in breast size, shape or texture, especially when comparing one breast to the other
- Swelling – a change in the size or contour of the breast
- Pain – any kind of tenderness or discomfort lasting more than a few days, including aching, burning, prickly sensation, or sharp pain
- Nipple changes – differences in the shape or position of the nipples, nipple inversion, or crustiness on the nipple or skin around it
- Discharge from the nipple that stains your bra/clothing without squeezing, especially if blood-stained
- Lump in your breasts or armpit
If you notice any change in your breasts, get yourself checked by a doctor as soon as possible to rule out anything serious that might need investigating.
When to see a doctor?
Never ignore a change to your breasts. It’s usually nothing serious, but getting checked is the only way to be sure.
If you notice any breast changes, contact your doctor straight away. This includes lumps, skin or nipple changes, or pain in your breasts that doesn’t go away. They’ll check your breasts and refer you to the specialist, so that you can get the care you need.
You can contact your doctor or visit one of our One Stop Breast Clinics where you can book a same-day diagnostic appointment, including a mammogram and/or ultrasound, and discuss the findings with a specialist breast surgeon on the same day.
One Stop Breast Clinic
At our One Stop Breast Clinics, you can get fast, direct access to an assessment with an expert breast consultant, a mammogram and a result on the same day.
Types of breast cancer
If you are found to have breast cancer, it could either be non-invasive (also known as DCIS), invasive, or metastatic.
Non-invasive breast cancer
About one in five women diagnosed with breast cancer through screening has non-invasive breast cancer. This means the cancer cells are only inside the milk ducts, called ductal carcinoma in situ (DCIS).
It’s the earliest form of breast cancer and is sometimes referred to as Stage 0, or pre-invasive or non-invasive cancer. If left untreated, the cells may begin to change, divide, and grow abnormally, eventually becoming an invasive breast cancer.
But when treated with surgery, DCIS usually doesn’t return or ever progress to a more invasive stage. So, finding and treating DCIS early almost always means a good outlook.
Invasive breast cancer
Invasive breast cancer is the most common form of breast cancer diagnosed by screening and in people presenting with symptoms. Most cases are treatable and diagnosed at early stages.
Early invasive breast cancer is when the cancer has grown into the breast tissue surrounding the ducts or lobes where it started. It’s only found in the breast or nearby lymph nodes and hasn’t spread elsewhere in the body.
There are two main types:
- Invasive ductal breast cancer – cancer that begins in the milk ducts and then spreads into the surrounding breast tissue
- Invasive lobular breast cancer – cancer that begins in the lobes (the milk-producing glands) and then spreads into the surrounding breast tissue
Sometimes, breast cancer cells don’t have any particular features when looked at under a microscope. This is called NST – which means ‘no special type’.
Inflammatory breast cancer is a less common invasive cancer where breast cancer cells have spread to lymph vessels in the skin. Skin symptoms of this can sometimes be misdiagnosed as breast infection. This is an aggressive type of cancer and is usually treated with systemic therapy first.
If left untreated, most invasive breast cancers will progress and spread elsewhere in the body.
Metastatic breast cancer
Metastatic breast cancer is when the cancer has spread outside of the breasts to other parts of the body, such as the bones, brain, liver, or lungs. This is also called advanced, stage 4, or secondary breast cancer.
Breast cancer types according to receptors
Your consultant will tell you the receptor status of your cancer cells, including HER2, oestrogen (ER), and sometimes the progesterone (PR) receptor status. This will help decide your treatment.
Your cancer could be:
- HER2 negative or HER2 positive (Human Epidermal Growth Factor Receptor 2)
- ER-negative or ER-positive (Estrogen Receptor)
- PR negative or PR positive (Progesterone Receptor)
The most common type of breast cancer is ER/PR positive and HER2 negative.
If your cancer is missing all three types of hormone receptors, it’s called triple-negative breast cancer.
What causes breast cancer?
Several risk factors influence your likelihood of getting breast cancer. Knowing your risk can help you to decide if you want to get more regular mammograms or consider lifestyle changes.
You’re more at risk of getting breast cancer if you:
- Are older – your risk increases with age, with four in five cases occurring in women over the age of 50
- Have a family history of breast or ovarian cancer – versions of the BRCA1 and BRCA2 genes can be passed on from parent to child and can increase your risk of developing breast cancer
- Have a certain lifestyle – such as drinking alcohol regularly, or being overweight or obese
- Have dense breast tissue
- Have been taking hormone replacement therapy for more than five years
- Have previously had breast cancer
Diagnosis and tests
How is breast cancer diagnosed?
The first step to finding breast cancer is either through screening or by having further tests to investigate a breast symptom, like a lump.
Screening for breast cancer is when you are checked for cancer even though you don’t have any signs or symptoms. The main way to screen for breast cancer is a mammogram, which is an X-ray.
If you have signs of breast cancer, such as breast changes noticed by yourself or picked up by a mammogram, the next step is to have further tests, such as an ultrasound, MRI, and biopsy.
Diagnostic tests assess whether your breast changes are benign (non-cancerous), like a cyst or benign tumour, or whether they are caused by breast cancer.
Diagnostics used for breast cancer include:
- Mammogram – a scan usually offered to women above 40 years of age and helps to screen both breasts for any abnormality
- A breast ultrasound – a scan to assess breast changes to determine the nature of lump and to decide if a biopsy is needed
- A biopsy – takes a very small sample of tissue from a breast lump to look for cancer cells under a microscope
- A breast MRI – the need for breast MRI will be determined by the specialist. One in two people has dense breasts, and for these people, a breast MRI is more effective than a mammogram for finding breast changes
Call us today
Stages of breast cancer
Your consultant will share your diagnosis with you and carefully explain the findings.
They’ll tell you:
- The type of breast cancer you have
- The size of the tumour, or tumours if there is more than one
- The grade of your cancer – this is how fast it’s growing scored on a scale of 1, 2 or 3
- The stage – which describes whether the cancer has spread and to what extent, scored on a scale of 0, 1, 2, 3, or 4
Breast cancer stages
Stage 0 | Also called ductal in-situ carcinoma, or non-invasive cancer. Precancerous cells that are only found in the milk ducts. |
Stage 1 | Also called early stage invasive breast cancer. The cancer is small and only in the breasts or nearby lymph nodes. |
Stage 2 | Also called early stage invasive breast cancer. The cancer is only in the breasts or nearby lymph nodes, or both. |
Stage 3 | Also called locally advanced breast cancer. The cancer is in the breast and the lymph nodes, breast skin or chest wall. |
Stage 4 | Also called secondary breast cancer, advanced breast cancer, or metastatic breast cancer. The cancer has spread elsewhere in the body. |
Breast cancer treatment overview
How is breast cancer treated?
There are several treatment options for breast cancer, which depend on the type, stage, and grade of cancer, as well as your overall health and personal treatment preferences.
Treatment can be personalised by considering your risk of cancer coming back after treatment. Genomic assays help predict the likelihood of recurrence, to help decide how intensive treatment should be.
Treatments for breast cancer include:
- Surgery, including breast-conserving surgery, is offered through our partner hospitals and is usually the first step in treatment
- Radiotherapy, which is usually done after surgery to either try to cure the cancer completely; reduce the risk of the cancer coming back after surgery; or, rarely, relieve symptoms if a cure is not possible.
- Chemotherapy, which is given as the first treatment for certain types of cancer, or after surgery for other types, to destroy any cancer cells that might have spread
- Endocrine (hormone) therapy to reduce the risk of cancer returning
- Targeted therapies, including monoclonal antibodies and immunotherapy
The treatment is personalised to you and your cancer. You and your specialist will review your options after a multidisciplinary team (MDT) has met to discuss a dedicated plan for you.
Learn more about our treatments for every type of breast cancer.
Prevention of breast cancer
Not every risk factor for breast cancer can be avoided, but Cancer Research UK suggests that one of every four cases has a preventable cause.
For example:
- Almost 1 in 10 breast cancers are related to being overweight or obese
- Almost 1 in 10 breast cancers are related to alcohol intake
Certain lifestyle changes can help lower your risk:
- Staying within your healthy weight range (BMI 18.5 - 24.9)
- Keeping your alcohol intake with recommended limits
- Avoiding smoking
Alongside this, you can give yourself the best chance of finding breast cancer early and having good outcomes by:
- Regularly checking your breasts for any changes
- Attending mammograms when you’re invited
- Getting checked by a doctor as soon as you notice any changes or differences in your breasts
Support at GenesisCare
From first symptoms through to advanced (secondary) breast cancer, we offer world-class breast cancer treatment and care tailored to every patient.
We equip our centres with the latest technologies and offer many of the newest breast cancer tests, scans and treatments that are proven to be safe and effective, as standard.
Our consultants are regional and national cancer experts who focus on you to achieve the best outcome possible and reduce the negative impact of treatment.
With us, you’ll receive the very best personalised care and a treatment plan that also embraces lifestyle-modifying approaches through our integrative cancer care programme, including exercise medicine and wellbeing therapies
Call us today
FAQs about breast cancer
How long does it take for breast cancer to spread?
One of the main challenges with cancer is that there’s a large variety in how it develops – in other words, every person is different. It’s not possible to predict with complete accuracy how an individual cancer will behave, including how fast it grows and whether it spreads.
Whether breast cancer spreads and how quickly depends on lots of factors. First, the breast cancer cells need to break away and spread through the blood or lymphatic system, without being destroyed by the immune system.
Once a breast cancer cell arrives in a new organ, like the lungs or brain, it often lies dormant for many years, meaning it doesn’t grow or change. It can stay dormant for decades. Researchers aren’t sure yet what might trigger these cells to start growing into metastases.
The main takeaway, though, is that regular screenings and prompt treatment can significantly improve outcomes in breast cancer by preventing or delaying how fast it spreads.
What does a breast cancer lump feel like?
Any breast lump should be checked as soon as possible by a doctor. Never try to self-diagnose whether a lump is cancer or not.
A breast cancer lump may feel like:
- A hard, firm and solid lump, like a seed
- A “shelf” beneath the skin
- A swollen breast or change in shape
Tumours in the lymph nodes or milk lobes can feel softer, like peas or kidney beans.
The lump might be ‘immovable’, which means it feels fixed and hard to move, or have ‘irregular edges’, meaning it doesn’t feel smooth.
Breast cancer lumps can be painless, or have sensations like an ache, burning, tingling, tenderness or pain.
Not all lumps mean cancer, but they should always be checked by a health professional to rule out anything serious that needs investigating
Can men get breast cancer?
Though most common in women, men can also develop breast cancer in rare cases, as it grows in the small amount of breast tissue behind a man’s nipples.
People of all genders, including men, women, trans people and non-binary people should look out for the same symptoms and see a doctor as soon as possible about any changes to their breasts or chest.
What is the survival rate for breast cancer?
Survival rates for breast cancer show how many people, on average, are still alive after their diagnosis at set time points, for example, 1 year, 5 years, and 10 years.
These statistics are based on data from a wide range of people of different ages, different subtypes of breast cancer, and different treatments. They’re generalised statistics and don’t necessarily predict what your outcome will be.
Recent statistics from Cancer Research UK show that:
- Almost everyone diagnosed with stage one breast cancer lives for five years or more (almost 100%)
- 90 in 100 people diagnosed with stage two breast cancer lives for five years or more
- 70 in 100 people diagnosed with stage three breast cancer lives for five years or more
- 25 in 100 people diagnosed with stage four breast cancer lives for five years or more
Overall, survival outcomes are good for people diagnosed with breast cancer in the UK, which is likely because of screening and early detection, and improvements in treatment options.
If you’ve been diagnosed with breast cancer, talk to your doctor about what’s the most likely outcome for you. They’ll be able to share more advice based on your personal circumstances.
Reviewed by:
Professor P.G. Roy
Consultant Oncoplastic Breast Surgeon
August 2024






