Optimising local control of Brain Metastases with Stereotactic Radiosurgery
With the rapid improvements in systemic therapy and extra-cranial stereotactic techniques we have seen over the last few years, optimal control of brain metastases has become even more important. Systemic treatment can be seen as “WBRT for microscopic disease” with SRS acting as a boost to the visible disease.
GenesisCare has therefore implemented new technologies, protocols and pathways to ensure that patients and referrers have access to all possible surgical and radiotherapy options – including a state-of-the-art Gamma Knife Icon at the GenesisCare centre for radiotherapy at Cromwell Hospital.
Our Neuro-Oncology team made up of leading UK Neurosurgeons, Neuroradiologists and Clinical Oncologists offers rapid, expert advice through a bi-weekly online MDT, working in collaboration with the referrer to ensure careful coordination with planned systemic and other therapies. Below is a case report, an overview of the evidence, and an idea of what the future has in store.
Clinical Case
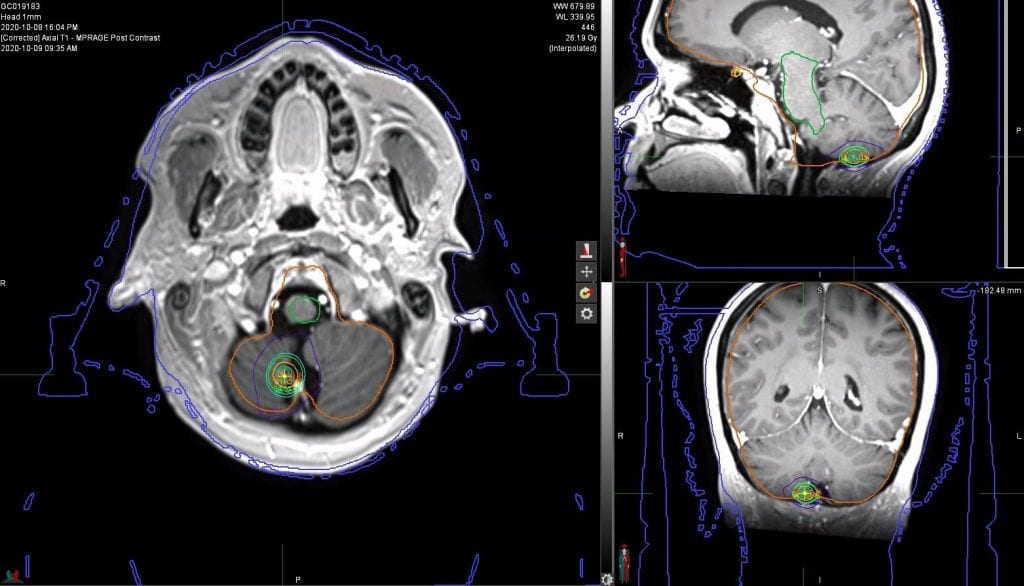
A 37-year-old lady with a diagnosis of metastatic adenocarcinoma of the lung (EGFR mutation positive (Exon 19 deletion)) with brain, node and ovarian metastases since 2018 had previously been treated with WBRT in 2019 followed by Carboplatin/Paclitaxel, which was stopped due to toxicity. She was switched to Osimertinib in February 2019. MRI head in September 2020 showed a new solitary brain metastasis in the right cerebellum with a PET scan showing stable extra-cranial disease. The patient was treated at GenesisCare in Oxford with SRS and, currently remains well and symptom-free. Follow up imaging showed a very good radiological response at six months.
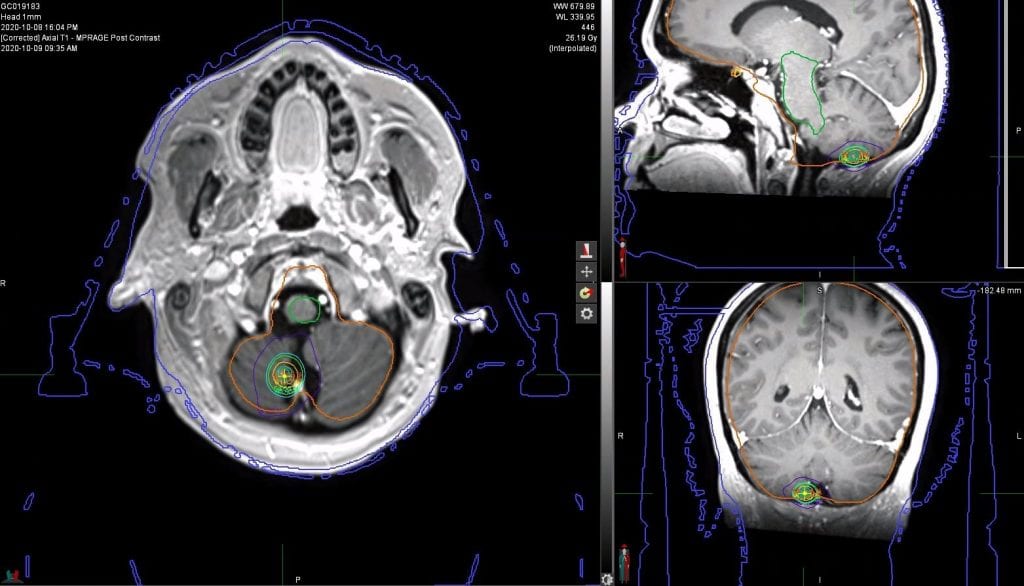
Figure 1. Isodose coverage of right cerebellar metastases (axial, sagittal and coronal views).
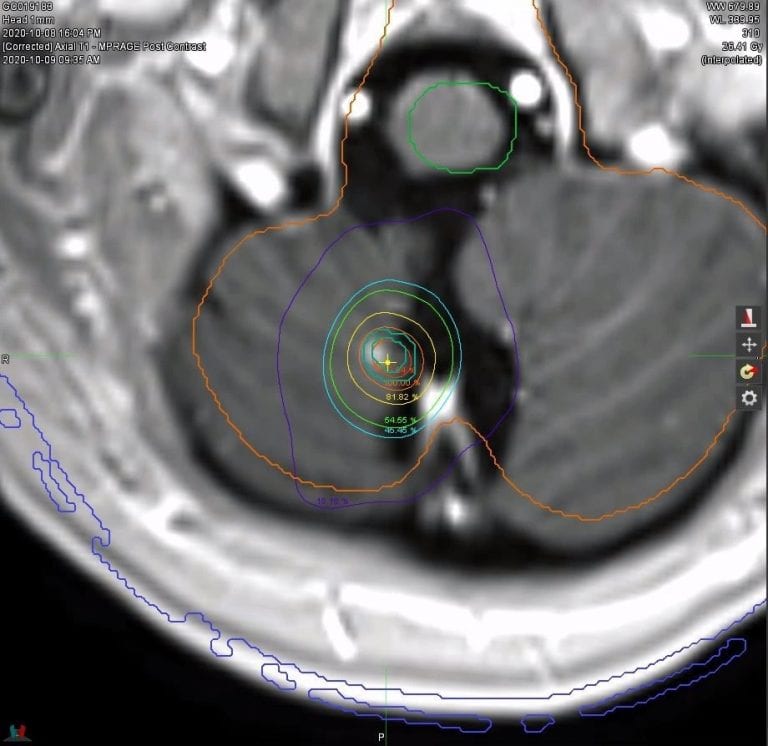
Figure 2. Isodose coverage magnified to highlight excellent PTv coverage and steep fall-off.
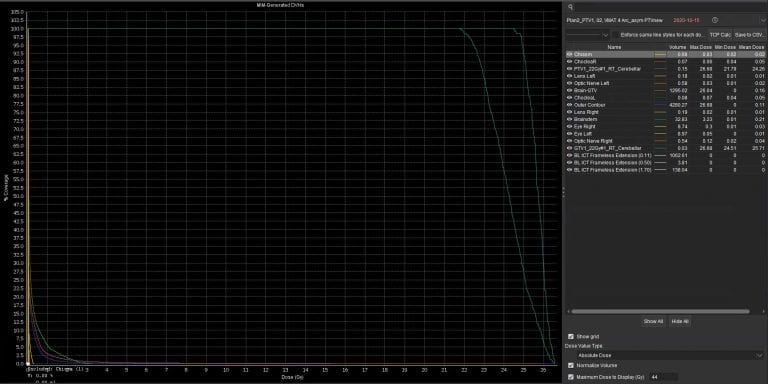
Figure 3. Dose-Volume Histogram for tumour and Organs at Risk (OAR)
Brain metastases management
Brain metastases occur in 30% of cancer patients with a median survival historically between 4 and 7 months, depending on prognostic factors, when treated with whole brain radiotherapy. Most systemic therapies are not effective in the brain, or only partially. Therefore, more local aggressive approaches to treat brain metastases are warranted. SRS is an ablative local treatment, alongside surgery, that makes it possible to treat multiple or otherwise challenging lesions, as well as consolidate surgical debulking. SRS is preferred to surgery in most cases where no histology is required, multiple metastases, or tumours in eloquent areas.
Scientific evidence supporting effectiveness of SRS in multiple brain metastases
SRS has proven ability to achieve local control at 1 year in 70-90%. SRS has been proven with level of evidence to increase overall survival and quality of life (1,2). Yamamoto et al (3) showed that there was no overall survival difference when treating 2-4 vs 5-10 brain metastases with SRS, concluding that SRS is preferred to WBRT when there are multiple brain metastases. A recent study (4) also found that there was no difference in overall survival (OS) when treating 2-4 vs 5-15 brain metastases with SRS.
SRS also has better neurocognitive outcomes. At ASTRO 2020, Ludmir et al (5) proved that SRS was associated with reduced risk of neurocognitive deterioration relative to WBRT without compromising OS. These results provided level 1 evidence to support the use of SRS in patients with 4-15 metastases.
Controversies and future directions
How many metastases should be treated with SRS?
Scientific literature supports that any number, provided the total PTV volume is less than 20 cc.
When there are brain metastases and patient is on systemic treatment that crosses the blood-brain barrier. Should we treat with SRS or hold it in reserve?
There are two options to be discussed in a multidisciplinary setting: to treat at the point the diagnosis is made, or wait until there are symptoms or the metastases progress.
Is WBRT an old-fashioned treatment?
WBRT has shown poor local control and overall survival with increased neurocognitive impairment, decreasing quality of life. The role of WBRT has become increasingly narrow given the new systemic therapies with effectiveness in brain and the increasing use of SRS in patients with limited number of metastases.
Do we have to stop systemic treatments during SRS?
It depends the type of treatment the patient is on. Immunotherapy can be kept during SRS, Targeted therapy should be stopped 3 days before and after SRS, and chemotherapy should be stopped 7 days before and after.
If you would like more information about how to access these treatments for your patients, please contact GCLO@genesiscare.co.uk.
Kind regards,
Dr Luis Aznar Garcia
Clinical Oncologist and Specialist Advisor SRS service