Review Date: September 2024
- Patients
- Exploring cancer care
- Conditions we treat
- Prostate cancer
What is prostate cancer?
About prostate cancer
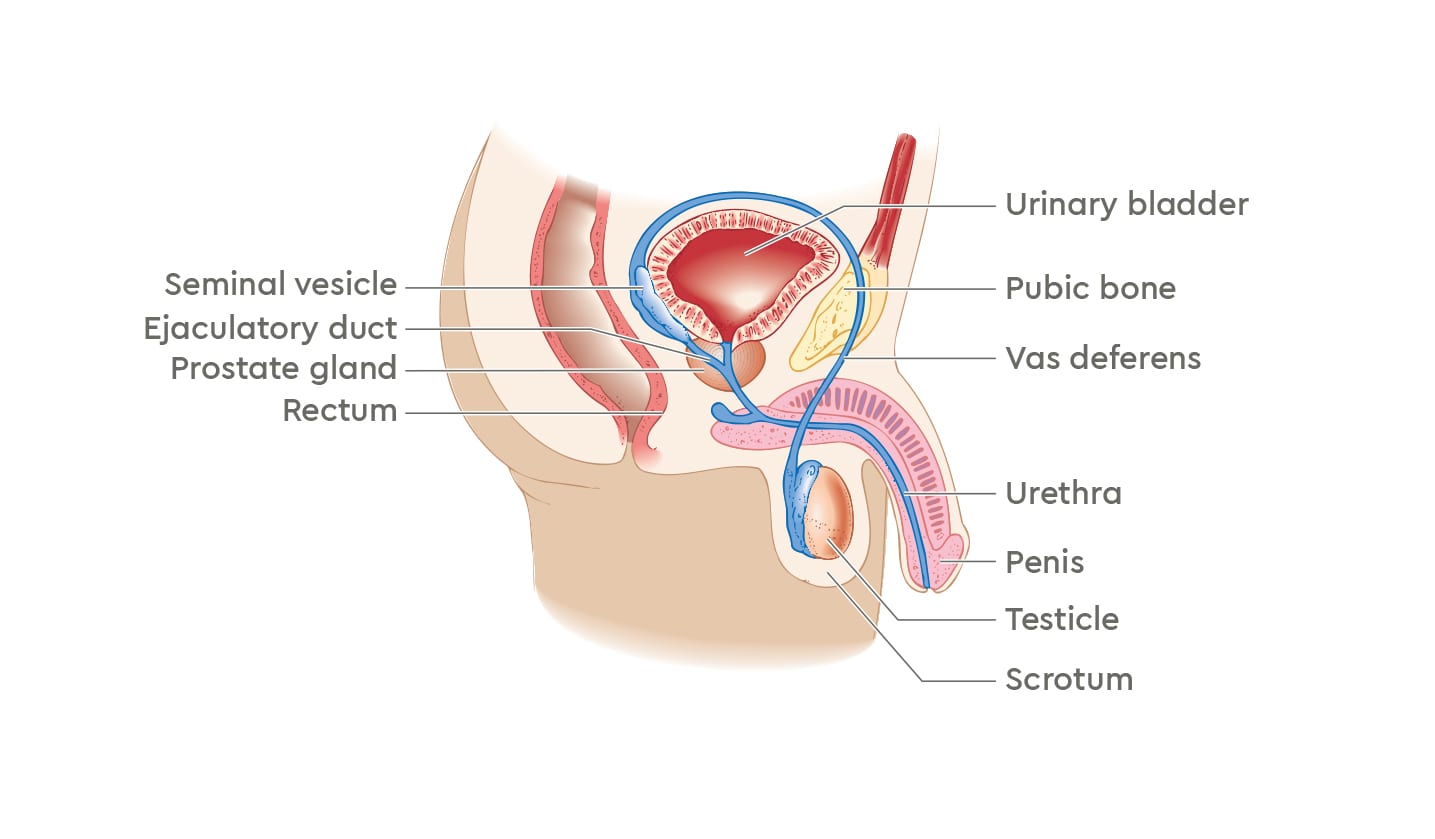
The prostate is a small gland that sits just below the bladder and in front of the rectum in men. It surrounds the urethra (the tube through the penis that takes urine and semen out of the body). The prostate gland is part of the male reproductive system. It makes prostate fluid, one of the parts of semen, and a protein called prostate specific antigen (PSA).2
The prostate gland is often described as being the size of a walnut, and it is normal for it to grow as men age. To grow and develop, the prostate relies on the male hormone testosterone, which is made by the testicles.2
Prostate cancer was the most commonly diagnosed cancer in Australia in 2018 and is estimated to remain the most commonly diagnosed cancer in 2022.1
Prostate cancer happens when abnormal cells in the prostate start to grow in an uncontrolled way. These abnormal cells may spread beyond the prostate. Prostate cancer can be described as:2,3
- Localised or early – where the cancer is only in the prostate
- Locally advanced – where the cancer has spread to areas near the prostate, such as the bladder, rectum, or pelvic wall
- Advanced or metastatic – where the cancer has spread to parts of the body further away from the prostate, such as the lymph nodes or bone
Prostate cancer may be slow growing, and many men with prostate cancer experience no or few symptoms and may live many years without the cancer spreading.2,3
Most men with early or localised prostate cancer do not experience any symptoms. Prostate cancer may not cause symptoms even when the cancer has spread. Symptoms that may occur with prostate cancer include:2,3
- Feeling frequent or sudden need to urinate
- Difficulty and/or discomfort when urinating
- Blood in semen or urine
- Pain in the lower back, upper thighs, or hips
- Unexpected weight loss
These are not all the possible symptoms of prostate cancer and are not always symptoms of prostate cancer. Symptoms and their severity will vary between individuals. Some symptoms may be difficult to notice.2,3
The exact cause of prostate cancer is not known, although there are some factors that are known to increase the risk of developing prostate cancer. Risk factors for prostate cancer include:1,2
- Age – risk increases rapidly after the age of 50 years
- Family history – risk is higher in men with a father or brother with prostate cancer
- Certain gene changes that can be inherited – BRCA gene mutations (associated with breast and ovarian cancers) can increase risk of prostate cancer
If you think you may be experiencing prostate cancer symptoms or have any questions about prostate cancer or your risk of developing it, speak to your doctor.
Make an enquiry
Contact us today to find out how GenesisCare can help you.
Diagnosis
Diagnosis
A number of different tests can be used to check for changes in the prostate and confirm a diagnosis of prostate cancer. Some of these tests include:2,3
- Blood test to check for raised levels of PSA – the PSA level can give an idea whether prostate cancer is likely or unlikely, but many factors can affect PSA levels so this test alone cannot diagnose prostate cancer and is usually used to help guide further testing
- Digital rectal examination (DRE) – a urologist uses a finger placed into the rectum to feel for changes in the shape or hardness of the prostate
- Magnetic resonance imaging (MRI) – a scan that takes detailed images of the inside of the body to find any changes in the prostate or other parts of the body
- Biopsy – uses a needle guided by ultrasound to take small samples of prostate tissue, which are examined under a microscope to confirm whether the cells are cancerous (malignant) or non-cancerous (benign).
If you are diagnosed with prostate cancer, your treatment and care will usually be provided by a group of different health professionals – called a multidisciplinary team (MDT). The specialist leading your treatment may be a urologist, a radiation oncologist, or perhaps a medical oncologist.1,2
Different factors influence the treatment plan that may be recommended for your prostate cancer, including:1,2
- Location of the cancer
- How advanced the cancer is
- How severe any symptoms are
- Your age and general health
- Your personal preferences
Making the decision about what cancer treatment to have may be difficult. We recommend you discuss all your options – including those suggested by your multidisciplinary team – with your specialist before starting any treatment. Some important considerations may include the location of the treatment centre, the duration of treatment(s), potential side effects, and any extra costs that may be involved.2

Find a doctor
Search for Prostate Cancer specialists in your state
Treatment options
Prostate cancer treatment options
Radiation therapy, also called radiotherapy, helps to kill cancer cells. Radiation therapy uses controlled doses of radiation to damage or destroy cancer cells, and can be delivered from outside the body (called external beam radiation therapy, or EBRT) or from inside the body (called brachytherapy).2,3
Radiation therapy may be offered in the early stages of cancer treatment, or after it has started to spread. There are different radiation therapy techniques that may be suitable for different cancer types at different stages.2,3
Radiation therapy techniques
Intensity Modulated Radiotherapy (IMRT) helps precisely deliver high doses of radiation to the tumour whilst protecting normal tissues, resulting in fewer side effects.4
Image Guided Radiation Therapy (IGRT) uses imaging (x-rays and scans) before and during treatment to track the exact shape, size, and location of the tumour, allowing for adjustments during treatment sessions to precisely target the tumour.4
Stereotactic ablative radiation therapy (SABR) uses modern 3D camera technology aiming to target and help kill cancer cells. The aim of SABR is to target tumours in the body with high doses of radiation therapy. It helps to destroy cancer cells with minimum damage to surrounding healthy tissues;10
- It’s often used to treat small tumours of the brain
- It’s accurate to within one to two millimetres
Stereotactic Body Radiation Therapy (SBRT) delivers high doses of radiation from many angles, allowing treatment of small tumours. SBRT can deliver a high dose of radiation over a shorter period, meaning fewer sessions and treatment duration (within clinics, not necessarily in hospitals).4
Low Dose Rate Brachytherapy (LDR) involves permanently placing brachytherapy seeds in, or near, the tumour inside the prostate. The seeds continually release low-dose radiation over several months.2,3
High Dose Rate Brachytherapy (HDR) is given by placing temporary needles or rods into the prostate under anaesthetic, and then delivering internal radiation, avoiding dose to the surrounding tissues.2,3
Volumetric Modulated Arc Therapy (VMAT) is a form of IMRT that uses a moving machine to shape the radiation to fit the target area, and usually involves shorter treatment sessions.4

Other treatments
Chemotherapy - uses medication to treat cancer by killing cancer cells or slowing their growth and spread. The medication is usually given intravenously (via a needle inserted into a vein). Chemotherapy may be used in conjunction with other cancer treatments. The type and duration of chemotherapy is determined on an individual basis by a patient’s medical oncologist.2,3
Theranostics - is an approach to cancer therapy that combines diagnostic and treatment techniques to detect and treat some cancer types. Theranostics may be used to treat cancers that have spread (metastasised), or where the cancer is advanced and/or has not responded to other treatments.8,9
Based on current research and clinical experience, theranostics is most likely to be suitable for patients with metastatic prostate cancer or neuroendocrine tumours.8,9 Your GenesisCare oncologist will determine if theranostics may be suitable for you.
Find a centre
Contact us today to find out how GenesisCare can help you.
Support services
Support services
Content reviewed by

- Cancer Council. Understanding Prostate Cancer. May 2024. Available: https://www.cancer.org.au/cancer-information/types-of-cancer/prostate-cancer [accessed June 2025].
- Cancer Australia. Prostate cancer. Available: https://www.canceraustralia.gov.au/cancer-types/prostate-cancer/overview [accessed October 2023].
- Prostate Cancer Foundation of Australia. Prostate cancer. A guide for newly-diagnosed men. November 2020. Available: https://www.pcfa.org.au/publications/information-resources/ [accessed October 2023].
- Cancer Council. Understanding Radiation Therapy. March 2024. Available: https://www.cancer.org.au/cancer-information/treatment/radiation-therapy [accessed June 2025].
- Kurup G. J Med Phys 2010;35(2):62–64.
- Hall WA, et al. CA Cancer J Clin 2022;72:34–56.
- RadiologyInfo.org. Image-guided Radiation Therapy (IGRT) Available from: https://www.radiologyinfo.org/en/info/igrt (accessed June 2025).
- Gomes Marin JF, et al. Radiographics. 2020;40(6):1715–1740.
- Vu TM, et al. ANZ J Surg. 2022;92(11):2782–2783.
- Therapeutic Goods Administration. Special Access Scheme: Guidance for health practitioners accessing unapproved therapeutic goods. V1.0 January 2023.

You are leaving our website
You are now leaving our website. GenesisCare do not control this content and therefore are not responsible for its accuracy or reliability.
Disclaimer:
This website is provided for information purposes only. Nothing on this website is intended to be used as medical advice, or to diagnose, treat, cure or prevent any disease. It should not be used as a substitute for your own health professional's advice. Any medical procedure or treatment carries risks. Before proceeding with treatment, you should discuss the risks and benefits of the treatment with an appropriately qualified health practitioner. Individual treatment outcomes and experiences will vary.
