- Home
- Treatment options
- Radiation therapy
- Stereotactic ablative radiation therapy SABR

Stereotactic Ablative Radiation Therapy (SABR)
Learn more about SABR and its use as a radiation therapy treatment for certain cancer types.
SABR Radiation Therapy
Stereotactic Ablative Radiation Therapy (SABR) uses modern technology to target tumours with an accuracy of 1–2 millimetres. It delivers high doses of radiation to the cancer while limiting exposure to surrounding healthy organs, which helps reduce the risk of side effects.1,2
- SABR is used to treat a range of cancer types, including lung, prostate, liver, bone/spine, and kidney cancers. It is particularly suited to soft tissue tumours and those located in complex anatomy4
- In some cases, SABR can be an alternative to surgery for small to medium-sized cancers. This may avoid the need for an anaesthetic and the risks of an operation, especially for patients who are elderly, frail, or have other health concerns1,3
- Patients typically require 1–5 SABR treatment sessions; the specific number will depend on your individual circumstances1
Your treating doctor and care team will provide more details about SABR and whether it is suitable for your tumour type.
Image guidance for SABR
Imaging technology is an important consideration in the delivery of SABR, as it underpins the precision and safety of the treatment.
Because SABR requires millimetre accuracy, it relies on imaging just before treatment to ensure the target is hit precisely every time.4
Advanced imaging assists in:
- Tumour targeting with millimetre precision
- Motion tracking to account for breathing or internal organ movement
- Treatment adaption to adjust for changes in anatomy across treatment days
- Treatment verification to confirm positioning before each session
Types of imaging technology
Three main imaging types are typically used for SABR:
Stereoscopic X-Ray imaging, commonly used in CyberKnife treatment, is an early form of image guidance. It offers a good level of accuracy for positioning and target verification; however, it may have limitations in soft tissue visualisation.
In more recent years more advanced 3D and real-time imaging technologies have become available including:
- CBCT (Cone-Beam CT) – provides detailed 3D images of bones and surrounding soft tissues
- MRI-guided imaging – tracks soft tissue in real time with high clarity
CBCT technology is standard across all GenesisCare Linac machines and is used in IGRT (Image-Guided Radiation Therapy) and ART (Adaptive Radiation Therapy). Several GenesisCare locations also offer advanced MRI technology with soft tissue mapping.
Imaging comparison
In Stereoscopic X-ray imaging (the technology used for CyberKnife)27 only high-density objects are visible - such as bones and fiducial markers (for example, gold seed fiducial markers used in some prostate cancer treatments).
In Image A (below), you can see the gold seed fiducial markers appearing white.
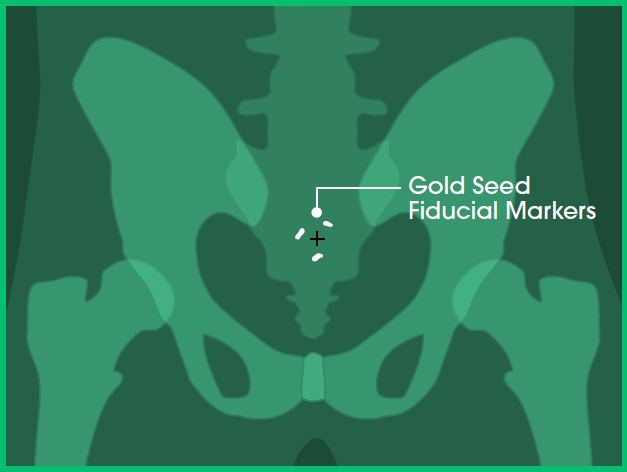
Image A: Front view
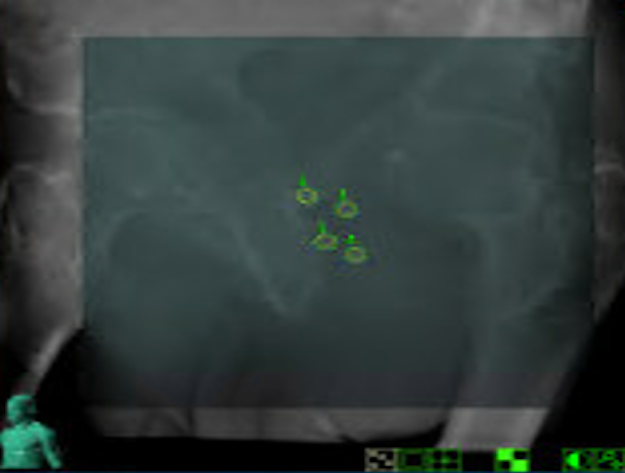
Image B: Clinical imaging scan
With Cone Beam Computed Tomography (CBCT), you can visualise a full 3D alignment of the patient and tumour with surrounding anatomy.
While high-density objects like bones and fiducial markers are still visible (as in stereoscopic X-ray), CBCT also allows you to view soft tissues in three dimensions.
In images A, B and C, you can see the:
- Prostate in red
- Bladder in blue
- Bowel in orange
- Fiducial markers in white
- Planned target volume outlined in yellow (where the radiation will hit)
In image D, which is an example of a CBCT, you can see the:
- Planned target volume outlined in blue
- Bowel outlined in orange
This level of imaging is standard at GenesisCare and is used in our Linac machines for Image-Guided Radiation Therapy (IGRT) and Adaptive Radiation Therapy (ART).
Note: Certain SABR treatments cannot be performed with stereoscopic imaging alone. Examples include targeting tumours or nodes in the chest, abdomen, or pelvis where critical healthy structures need to be visualised before delivering treatment that stereoscopic imaging cannot see.
Without knowing the tumour's position in relation to nearby healthy organs, there is a risk of overdosing healthy tissue, which may lead to side effects.
CBCT technology also enables real-time tumour tracking when combined with fiducials. It can capture images during treatment delivery, visualising fiducials within the tumour. This means treatment can be monitored in real time and paused if the tumour moves out of position.
This technology is standard for SABR treatment of prostate cancer.
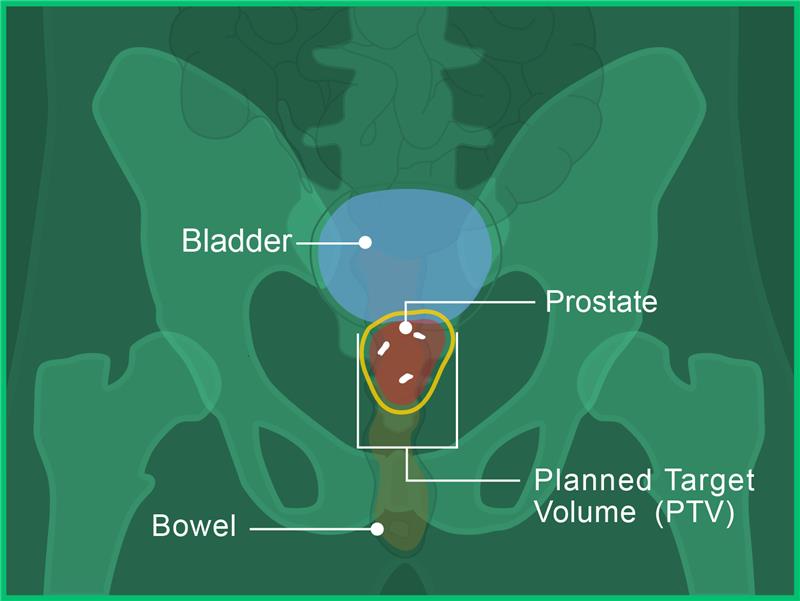
Image A: Front view
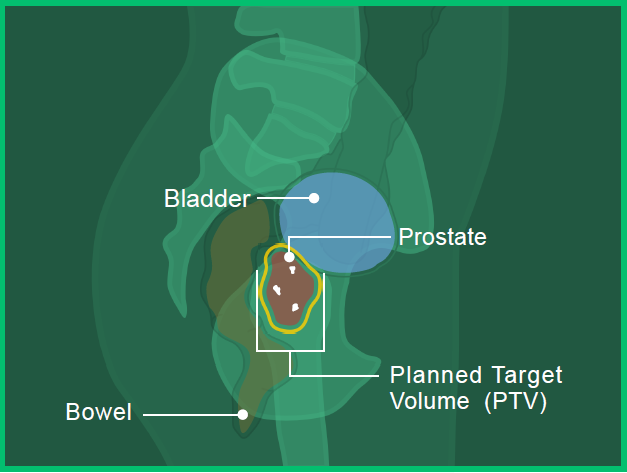
Image B: Side View
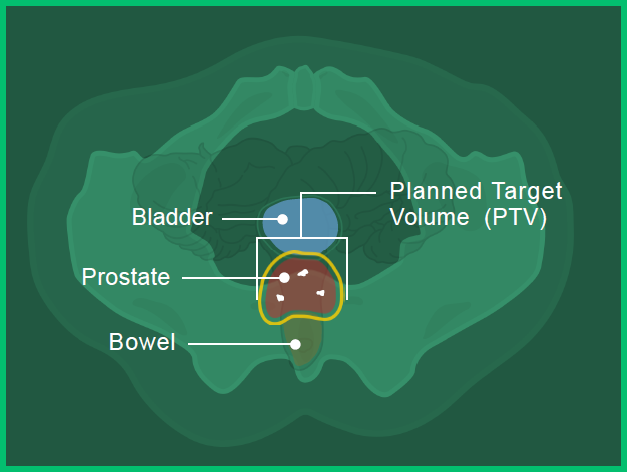
Image C: Bottom View
Image D: Clinical imaging scan
Magnetic Resonance Imaging (MRI) enables even more detailed visualisation of soft tissue, in addition to high-density objects.
In image A, you can see the:
- Prostate in red
- Bladder in blue
- Bowel in orange
- Fiducial marker in white
- Planned target volume outlined in yellow (where the radiation will hit)
Image B shows the high level of detail available with MRI-guided radiation therapy. You can see the:
- Planned target volume outlined in blue
- Bowel outlined in orange
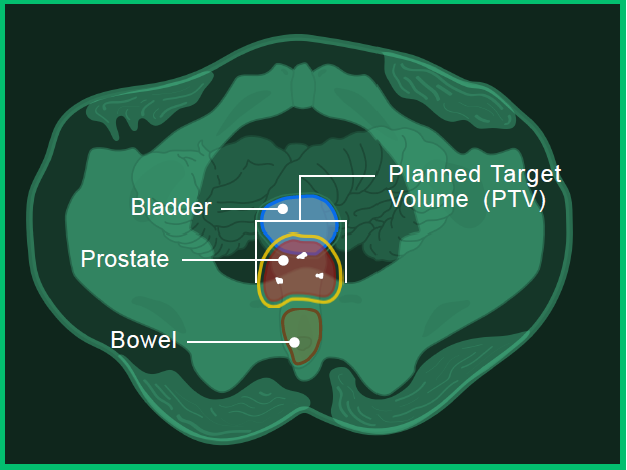
Image A: Bottom view
Image B: Clinical imaging scan
Find a centre near you
Read next

Our centres
In Australia, we have more than 40 oncology centres in metro and regional Queensland, New South Wales, Victoria, South Australia, and Western Australia.

Our doctors
Our experienced, specialised doctors offer bespoke, dedicated care aiming to provide the best possible clinical outcomes.

Radiation therapy for cancer
Radiation therapy uses high energy X-rays or other particles to treat cancer and can be used at all stages.
- Cancer Council. Understanding Radiation Therapy. Available at: https://www.cancer.org.au/assets/pdf/understanding-radiation-therapy-booklet (accessed June 2025).
- Tsang Maverick WK. Journal of Thoracic Disease 2016;8:S517–S527.
- Andruska N et al. Journal of Thoracic Oncology 2021;16:1075–85.
- Radiation Oncology Targeting Cancer. Stereotactic Ablative Radiotherapy in AU and NZ. Available from: https://www.targetingcancer.com.au/radiation-therapy/stereotactic-ablative-radiotherapy-sabr (accessed June 2025).
- Kurup G. J Med Phys 2010;35(2):62–64.
- Hall WA, et al. CA Cancer J Clin 2022;72:34–56.
- RadiologyInfo.org. Image-guided Radiation Therapy (IGRT) Available from: https://www.radiologyinfo.org/en/info/igrt (accessed June 2025).

You are leaving our website
You are now leaving our website. GenesisCare do not control this content and therefore are not responsible for its accuracy or reliability.
Disclaimer:
This website is provided for information purposes only. Nothing on this website is intended to be used as medical advice, or to diagnose, treat, cure or prevent any disease. It should not be used as a substitute for your own health professional's advice. Any medical procedure or treatment carries risks. Before proceeding with treatment, you should discuss the risks and benefits of the treatment with an appropriately qualified health practitioner. Individual treatment outcomes and experiences will vary.


