Prostate re-irradiation with MR linac based SABR
A SABR case study
Although external beam radiotherapy remains one of the main therapeutic options for the management of localised prostate cancer, biochemical recurrence occurs in 30-50% of patients (1). Standard of care for most patients is with lifelong androgen deprivation therapy (ADT) aimed at systemic disease control. Unfortunately, this is associated with long-term side effects that may significantly impact quality of life.
Twenty to 30% of all recurrences are due to intraprostatic disease alone, and may benefit from local salvage therapy (2, 3). However, only around 2% of recurrences are treated with local salvage therapies e.g., with salvage prostatectomy (4) and access to salvage options is often limited to specialised centres with the most experience.
Stereotactic ablative radiotherapy (SABR) is a form of precisely targeted radiotherapy. This allows for new opportunities to treat small targets with high radiation doses, bringing dosimetric and radiobiological advantages to the salvage treatment forum. Re-irradiation of the prostate with SABR aims to provide local control of the disease, and delay the need for indefinite ADT in the short and possibly, long term, while sparing the adjacent organs at risk (OARs)
In this emerging space, there are few, heterogenous, small, whole gland/focal prostate SABR re-irradiation series with limited follow up, prospective clinical trial data is lacking. Doses range from EQD2 44 to 82Gy (prostate α/β ratio= 2) in 5 to 6 fractions on alternate days. Reported toxicity has also been variable at up to 33% ≥Grade 2 GU and GI toxicity, but with only isolated reports of G3/4 toxicity. The incidence of GI toxicity is consistently lower than GU toxicity. Biochemical control rates are reported at between 50 and 83%, in this small group of studies with limited follow up (5,6,7,8,9).
Treatment on the MR linac allows optimal SABR treatment with daily assessment of the target and organs at risk, allowing recontouring and plan re-optimisation, and tracking of the target during treatment delivery.
LH is a 73-year-old man with a previous history of high-risk prostate cancer. He presented in 2006 with a PSA of 32, Gl 3+3, GG1 disease, radiological stage T3aN0M0. He was treated radically, with LHRH analogue treatment for a total of 2 years with concurrent three field conformal radiotherapy to the prostate and seminal vesicles, receiving 55Gy in 20 fractions, as was standard at this time. His hormone treatment was completed in 2008.
He represented in July 2020 with a raised PSA of 14 and a clinically flat, firm feeling prostate. His PSMA PET-CT scan demonstrated a markedly avid focus within the left mid-gland/base of the prostate and medial aspect of the left seminal vesicle (Figure 1). This was confirmed on a multi-parametric MRI (mpMRI) of his prostate. Systematic prostatic biopsies confirmed the presence of unilateral recurrent left sided prostate cancer.
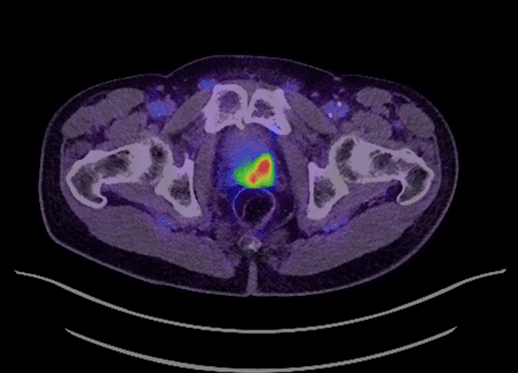
Figure 1 – PSMA PET/CT with avidity in left mid gland/base prostate and medial aspect of left seminal vesicle
He was keen to receive local treatment for his recurrent prostate cancer, avoiding indefinite ADT and its associated toxicities. He discussed radical prostatectomy with the urologists, but favoured treatment with SABR, as a less invasive option. He was consented, understanding the limited evidence for this approach.
Prior to radiotherapy, he had a rectal spacer placed to reduce the risk of significant rectal toxicity.
His previous radiotherapy treatment details were obtained and used to estimate the doses that could safely be given to his organs at risk (bladder, rectum, bowel, urethra), assuming maximal dose delivered previously, based on the time since his previous radiotherapy and tissue alpha/beta ratios. His GTV was defined using his mpMRI prostate and PSMA PET scan. A CTV was created from his GTV+2mm margin, adjusted to the prostate contour. PTV=CTV+2mm. He was treated with 35Gy in 5 fractions on alternate days.
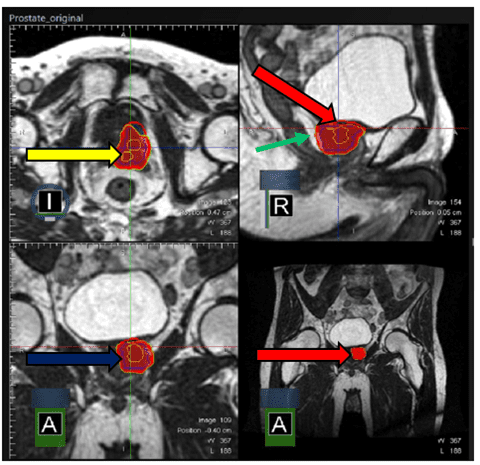
Figure 2 – Partial prostate treatment contours with 100% isodose
Key:
Yellow contour – GTV
Blue contour – CTV
Red contour – PTV
Red wash – 100% isodose with bladder sparing
Green arrow – rectal spacer
Treatment was planned (Figure 2) and delivered, with daily adaptation, consistently achieving coverage as planned of the planning target volume, while respecting the dose constraints of the OARs (Figure 3).
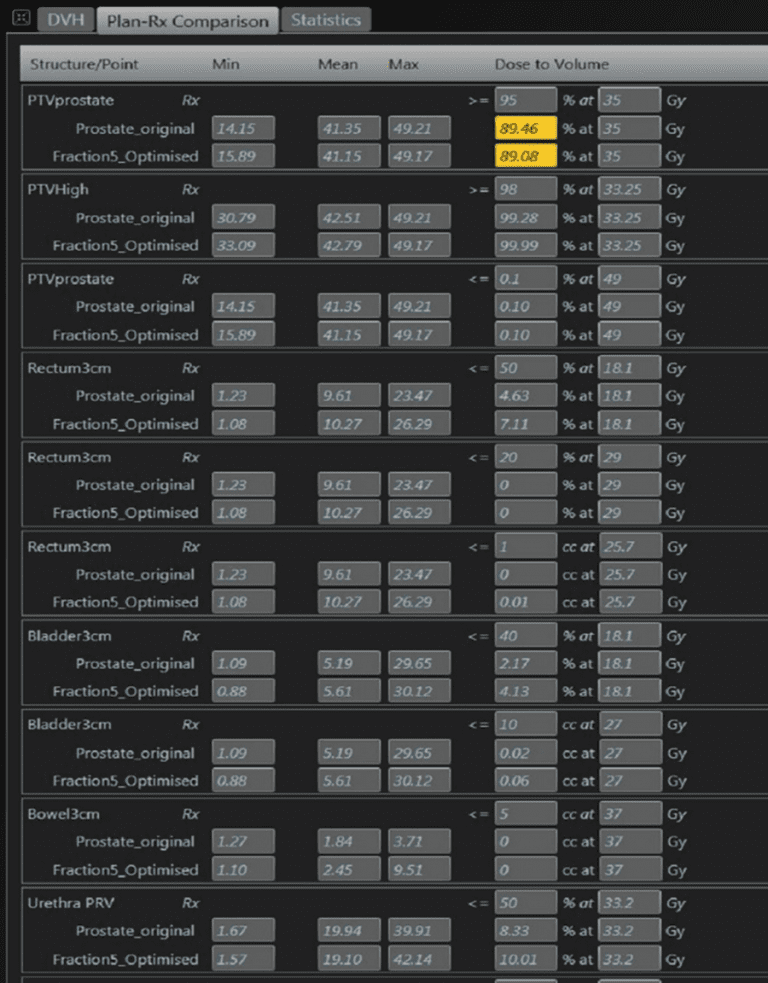
Figure 3 – Baseline and fraction 5 plan objectives
LH tolerated his treatment very well and has reported no toxicity at his end of treatment and 3-month review.
This case report illustrates that MRL based SABR re-irradiation of the prostate is feasible and safe in the short term, as has previously been reported. While long term prospective data is awaited, toxicity and outcome data from these case reports will continue to be collected as part of our registry.
If you would like more information about how to access these treatments for your patients, please do not hesitate to contact urologysat@genesiscare.co.uk
Kind regards,
Dr Ami Sabharwal
Clinical Oncologist and MRIdian Specialist





