SABR for spinal lesions
Stereotactic radiotherapy is a powerful tool for the control of spinal metastases. Here, SABR reference group member Dr Alex Martin reviews some of the latest evidence outlining the use of SABR for spinal lesions, with a focus on maximising safety.
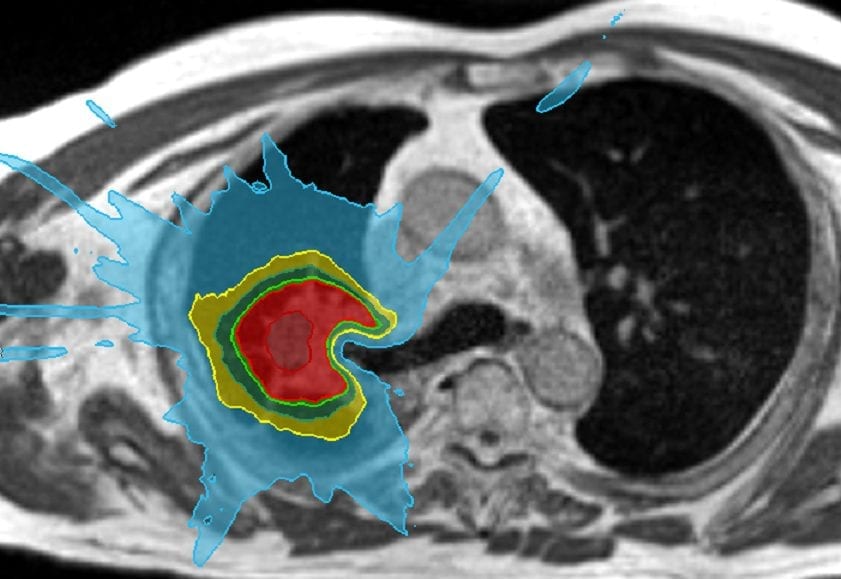
Spinal SABR poses the challenge of delivering an ablative tumour dose whilst staying within safe healthy tissue dose constraints.
The main focus in spinal SABR planning is the dose to spinal cord and cauda equina, since radiation myelopathy can have a huge impact on quality of life and prognosis. Thankfully with careful planning and delivery the incidence of myelopathy is low: a systematic review of SABR in previously untreated spinal metastases reported only 2 cases of neurological injury in over 1000 lesions treated. (1)
Perhaps less attention has been paid to the development of vertebral compression fracture (VCF) following spinal SABR, although it is a much more common late toxicity and can cause significant morbidity. The same systematic review reported a VCF in 9.4% of patients treated, of which 43% were new fractures and 57% were progression of existing fractures.(1) Other publications have reported new or progressing VCF in 14-20% of patients.(2),(3) Fractures usually develop/progress within a few months, but can appear up to a few years following treatment.
A number of risk factors for VCF post-SABR have been identified, including higher dose per fraction, lytic tumours, pre-existing fracture and spinal deformity.(4) In this month’s edition of the Green Journal, Chen et al 5 have looked at the relationship between SABR target dose/volumes and the risk of VCF in previously unirradiated patients. They analysed the treatment plans of 224 vertebral target volumes. CTVs were defined according to the ISRS consensus (6) (as per UK SABR Consortium Guidelines) with a 1-2mm PTV margin. Normal tissue complication probability (NTCP) modelling was used to explore the association between VCF risk and the dose to different sub-volumes of the PTV. They found that the dose to 80% of the PTV (D80%) was the best predictor of VCF risk, whereas the maximum dose (Dmax) and other small volume parameters did not show the same significant dose relationship. In other words, the dose to larger volumes of the vertebra is the best predictor of VCF risk rather than small areas of very high dose.
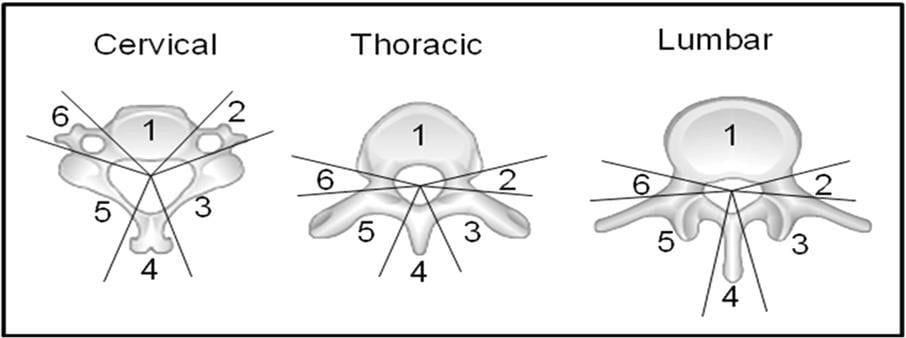
In general, dose escalation is likely to increase the risk of VCF, if other plan parameters are the same. On the other hand, prescribing to a higher isodose level (i.e. prescription isodose level higher than 70-80%) may reduce the risk by reducing the D80% dose. Unfortunately, this may in turn reduce the dose gradient outside the target, with implications on the dose to spinal cord. Another strategy would therefore be to try to reduce target volumes which would in turn reduce the dose to larger portions of the vertebra. The ISRS guidelines (6) divide the vertebra into segments (Figure 1) with instructions on when to involve adjacent segments, depending on the position and extent of the GTV. The rationale here is to avoid near-field disease relapse from tumour not adequately covered by the target volumes. However, it has in turn led to a significant increase in the target volumes for spinal SABR. The authors of the current paper argue that this approach could be refined in the future, perhaps with the use of novel imaging to improve tumour identification, and also Simultaneous Integrated Boost to the gross tumour.
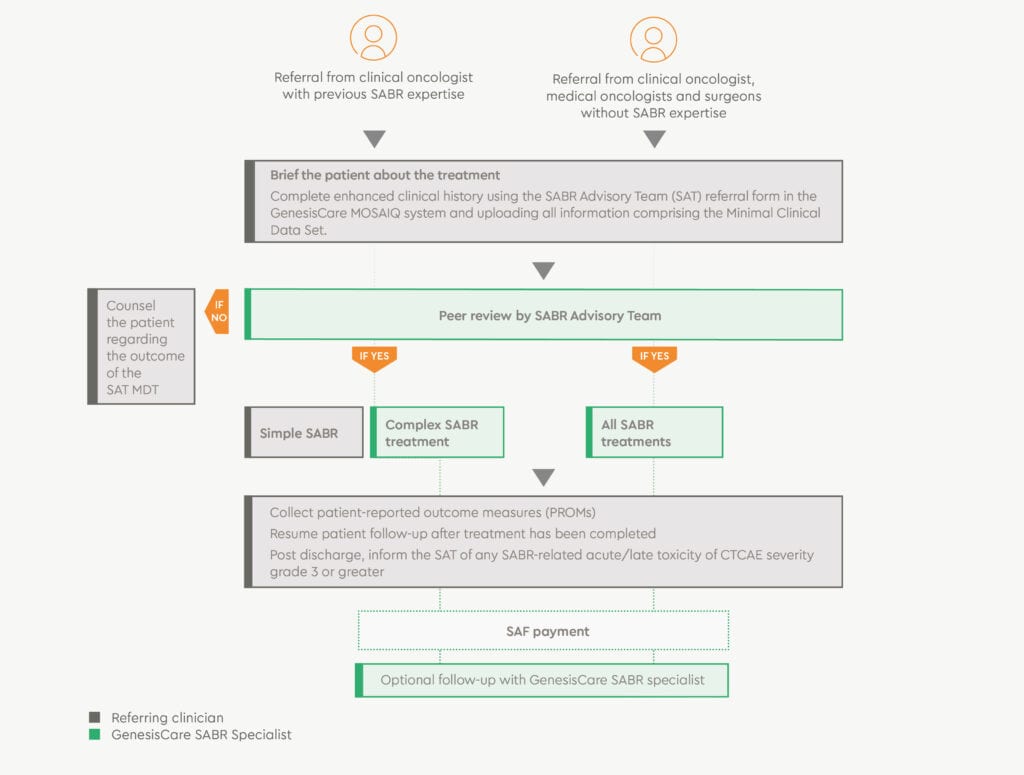
At GenesisCare, all potential patients will be reviewed in our twice-weekly virtual SABR MDT, and the SABR Advisory Team are available to offer peer review for all aspects of treatment planning. Treatment on the MR-linac is considered for patients with disease very close to the spinal cord, where reirradiation is needed, and where metalwork would make conventional SABR dosimetry challenging.
Figure 1. Anatomic classification system for consensus target volumes for spine SABR. (6)
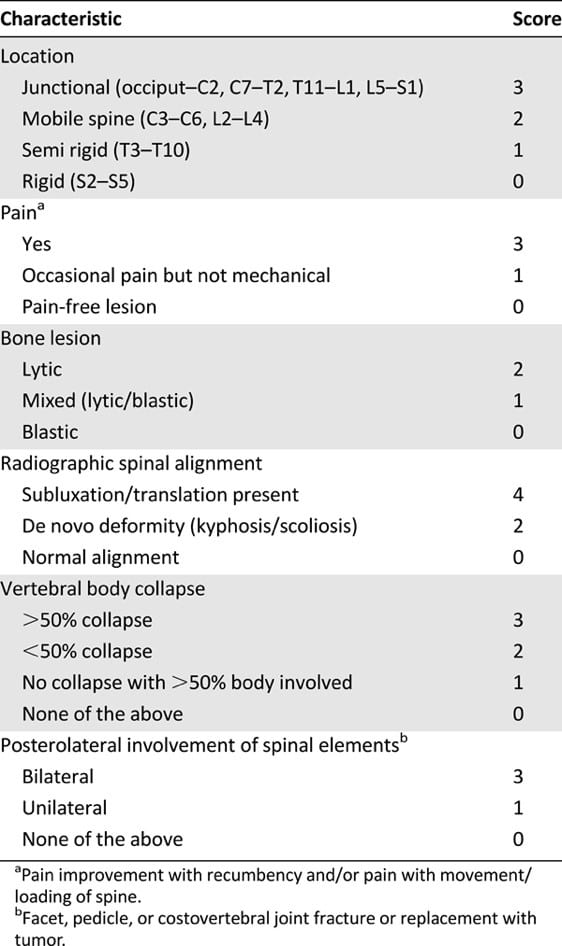
In the meantime, we should continue to use ISRS guidelines for CTV delineation, but need to be proactive in identifying patients at greater risk of VCF. The Spinal Instability Neoplastic Score (SINS) (Table 1) is well-validated and in the current paper was shown to correlate with VCF risk on multivariate analysis. (5) All potential spinal SABR patients should have a SINS calculated, usually with a diagnostic spine MRI to assist in accurate scoring. Patients with potential instability (score 7-12) should have a surgical assessment before proceeding with SABR, and those with a score of >12 should not be considered for SABR.
Table 1. Spinal Instability Neoplastic Score (SINS).
GenesisCare complex SABR referral process
- Check referral criteria | Counsel patient
- Complete referral form
- SABR coordinator uploads minimum dataset
- SAT review | Treating consultant selected
- SABR coordinator to PAO
- Patient informed of treatment plan
- Patient seen and treated
Eligibility criteria
- Histologically confirmed cancer
- ECOG PS 0-2 and able to lie in the treatment position
- In case of oligoprogressive disease, maximum of 3 metastases, and no more than 2 vertebral metastases
- No evidence of spinal cord or cauda equina compression
- Targets well-defined on imaging
- SINS score of
Minimum dataset
- SAT referral form
- Whole body imaging report and images within last 6 weeks
- MRI whole spine within 6 weeks
- Good organ function
- Referrers written report with full clinical history
- MRI contraindications
Read more information on SABR here.
Kind regards,
References:
- Husain Z A et al. Stereotactic body radiotherapy for de novo spinal metastases: systematic review. J Neurosurg Spine 27:295-302, 2017
- Boehling N S et al. Vertebral compression fracture risk after stereotactic body radiotherapy for spinal metastases. J Neurosurg Spine 17(4):379-386, 2012
- Tseng C-L et al. Imaging-Based Outcomes for 24Gy in 2 Daily Fractions for Patients with de Novo Spinal Metastases Treated with Spine Stereotactic Body Radiation Therapy (SBRT), Int J Radiat Oncol Biol Phys 102(3):499-507, 2018
- Sahgal A et al. Vertebral Compression Fracture After Spine Stereotactic Body Radiotherapy: A Multi-Institution Analysis With a Focus on Radiation Dose and the Spinal Instability Neoplastic Score. J Clin Oncol 31(27):3426-3431, 2013
- Chen X et al. Normal tissue complication probability of vertebral compression fracture after stereotactic body radiotherapy for de novo spine metastasis. Radiother Oncol 150:142-149, 2020
- Cox B W et al. International Spine Radiosurgery Consortium consensus guidelines for target volume definition in spinal stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 83(5):e597-605, 2012