Red flags for head and neck cancer in primary care
Early diagnosis of head and neck cancer is key
Head and neck cancer is the 8th most common cancer in the UK. There are over 12,000 new cases each year, and this number is rising1.
While curable when detected early, there is not one single sign or symptom that indicates head and neck cancer. This can make a diagnosis particularly challenging, especially in primary care. Patients can present with a neck lump or have less obvious symptoms such as hoarseness or voice changes, swallowing difficulties, a feeling of a lump in the throat or persistent mouth ulceration.
Prof. Stuart Winter and Mr Satheesh Prabhu are two of our consultant surgeons who provide assessment and diagnosis through our rapid access head and neck service at GenesisCare in Oxford. In a recent educational webinar, they outlined the red flags to help GPs identify and refer patients with suspected head and neck cancer.
Head and neck cancers
There are lots of areas within the head and neck where cancers can arise. To help identify potential signs of head and neck cancer, Mr Prabhu outlines six red flags for GPs to consider:
1. Ulcers
The oral cavity can be challenging to discern routine ulceration from malignancy. But, if you spot a persistent ulcer that has a hard margin, then this is a red flag for referral. Lip ulcers, often from sun exposure, are also red flags for referral.
2. Coloured areas in the mouth (erythroplakia or other coloured lesions)
Patches of red and white lesions in the mouth called (erythroplakia and leukoplakia) can also be a tell-tale sign of early-stage carcinoma. Some of these are pre-malignant but can become a cancer in up to 25% of cases.
However, GPs should equally be aware of other non-homogenous patches of lesions.
3. Floor of mouth lesions
With most head and neck cancers, a history of smoking and drinking increases the risk. This is relevant as most carcinogens end up on the floor of the mouth and, due to the location, lesions here are unlikely to be related to trauma.
Mr Prabhu urges GPs to have a low threshold for referral with floor of mouth lesions.
4. Lumps in the lip, oral cavity, neck, or thyroid
With regards to lip and oral cavity lumps, if a patient hasn’t reported recent trauma or dental work, this could well be a sign of carcinoma.
While only 1 in 20 neck lumps end up being cancer6, a patient presenting with a persistent or unexplained lump should be considered for referral.
5. Erosive lichen planus with white hue
In this scenario, it can be difficult to differentiate between erosive lichen planus and dysplasia, therefore Mr Prabhu advises referral, particularly if ulceration exists.
6. Patient-reported symptoms
Hoarseness, swallowing difficulties and burning sensations when eating spicy foods are all potential indicators but can be difficult to separate from other causes.
Here, as with all the other red flags, GPs should consider symptoms in the context of the patient’s history. NICE recommends referring on the basis that these symptoms are “persistent and unexplained”.
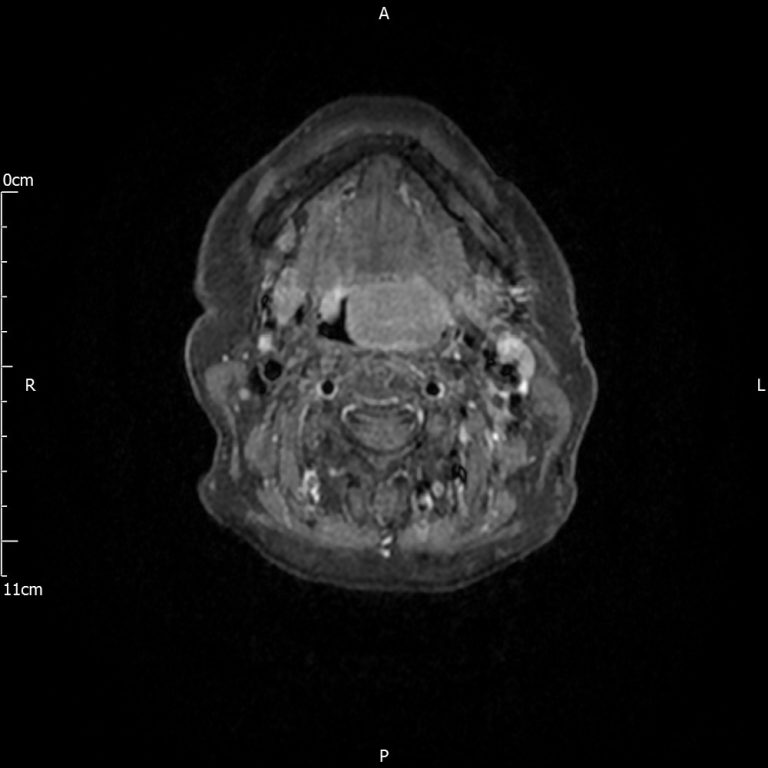
MRI scan of a patient with a large tongue base tumour who noticed a change in their swallowing

Picture of early laryngeal cancer picked up due to a change in voice
Timing is everything
Survival and quality of life in head and neck cancer are directly linked to the site and size of the primary tumour2.
The importance of catching these types of cancer early is reflected by the fact that the 5-year survival rate reduces from over 80% in locally diagnosed patients to less than 40% for those diagnosed at a late stage. However, in the last decade, less than a third of cases have been diagnosed.
Once detected, it is important that patients receive a speedy diagnosis and staging as well as discussion at a specialist tumour board.
Early detection and subsequent referral is therefore crucial to ensure the best possible outcomes.
At the beginning of October 2021, a study published in the British Medical Journal found that 6 out of 10 patients presenting to primary care with ‘red flag’ symptoms of possible cancer did not receive an urgent referral in the 14 days after presentation4, despite this being recommended in clinical guidelines.
A reluctance to refer is understandable – ear, nose and throat conditions make up 25–50% of all consultations5 and head and neck cancer symptoms could be confused with more common diagnoses.
Meanwhile, patients may notice symptoms but for a number of reasons may not seek immediate advice.
However, the effects of head and neck cancer are significant and carry serious implications from both a functional and psychological standpoint. Aside from a cancer prognosis, patients’ appearances, speech, and mental health are often affected, impacting patients’ quality of life.
Why wait two weeks to refer?
Head and neck cancers can have devastating effects on patients in terms of morbidity as well as mortality. That’s why at GenesisCare we recognise the importance of ensuring GPs are supported in knowing the symptoms to be aware of so they can refer at the earliest opportunity for diagnosis and treatment.
In the context of head and neck cancer, two weeks is a long time to see a specialist – so why wait?
At GenesisCare we’ve designed a rapid access head and neck service providing appointments often within 24 hours of referral for the fast assessment, diagnosis and treatment of patients referred from a primary care setting. With an easy GP referral process, it’s a real commitment to early diagnosis.
What’s more, GenesisCare offers world-class treatments including the most advanced radiotherapy techniques, such as volumetric modulated arc therapy (VMAT) and surface guided radiation therapy (SGRT) to their patients across the UK. This is supported by multidisciplinary teams consisting of speech and language therapists, dietitians and clinical nurse specialists to support patients throughout their treatment journey.
Find out more about our rapid access head and neck service and how to refer.
References
- Head and neck cancers statistics [Internet]. Cancer Research UK. 2021 [cited 27 October 2021].
- Gerstner A. Early detection in head and neck cancer – current state and future perspectives. GMS Curr Top Otorhinolaryngol Head Neck Surg [Internet]. 2008 [cited 27 October 2021];7:Doc06.
- Thompson‐Harvey A, Yetukuri M, Hansen A, Simpson M, Adjei Boakye E, Varvares M et al. Rising incidence of late‐stage head and neck cancer in the United States. Cancer. 2019;126(5):1090-1101.
- Wiering B, Lyratzopoulos G, Hamilton W, Campbell J, Abel G. Concordance with urgent referral guidelines in patients presenting with any of six ‘alarm’ features of possible cancer: a retrospective cohort study using linked primary care records. BMJ Quality & Safety. 2021;:bmjqs-2021-013425.
- Gardner S, Wijesekara J. ENT 2–Week Wait audit. British Journal of General Practice. 2009;59(567):779.3-780.
- Thyroid cancer – Symptoms [Internet]. nhs.uk. 2021 [cited 27 October 2021].
